About ACLF
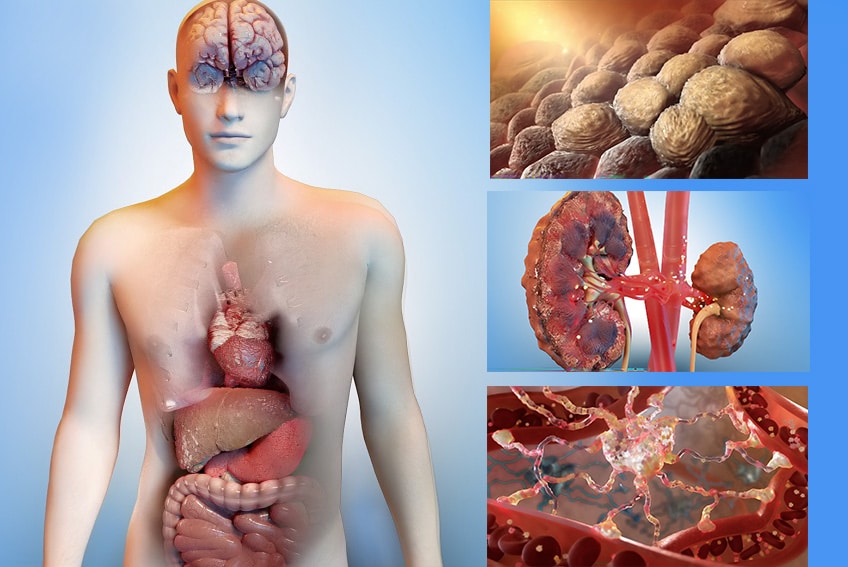
ACLF presents as a syndrome defined by a combination of hepatic and extrahepatic organ dysfunctions and failures and a uniformly poor prognosis. In patients with liver cirrhosis and acute hepatic decompensation, ACLF can be triggered by a precipitating event (e.g., an infection) that leads to a progressive functional deterioration of multiple organs with high short-term mortality (23% to 74% mortality at 28 days1).
In 2021, the prevalence of ACLF was estimated to be approximately 294,000 across the US, EU4, and UK2; a number expected to grow up to ~300,000 patients by 20362 . The incidence is growing at epidemic rates (+26% between 2006 and 2014) due to an aging population and a higher prevalence of steatotic liver disease3, diabetes, obesity, as well as alcohol consumption.
The management of ACLF results is a significant economic burden on healthcare systems, leading to a high need for innovative therapies. In the US, the average cost per hospitalization per patient amounts to $52,000.4 The overall estimated cost in the US in 2021 is $6.4 billion5 (a nearly 4-fold increase since 2011)

Unmet Needs
There are no specific therapies approved for patients with ACLF other than treatment of precipitating events (e.g., infection), when identified, and organ failure support. Liver transplantation remains the only treatment provided that an organ is available and the patient is eligible to receive it. 15-30%6 of patients die while awaiting liver transplant.
Thus, ACLF represents a high unmet medical need and a significant economic burden for healthcare systems.
Our ACLF Pipeline7: 5 Assets to Address ACLF and its Complications
Our ACLF pipeline is unique, with 5 assets in research and development, including those currently in Phase 2. VS-01, NTZ, SRT-015, CLM-022, and VS-02-HE are all based on differentiated mechanisms of actions leveraging complementary pathways.
VS-01-ACLF
VS-01-ACLF is an innovative, investigational drug based on a proprietary scavenging liposomal technology. It is administered directly into the peritoneal (abdominal) cavity following drainage (paracentesis) of ascites, one of the most common complications in patients with ACLF.
VS-01 has been granted Orphan Drug Designation (ODD) in ACLF by the US Food and Drug Administration (FDA). Given the high unmet needs in this indication, it is expected that the program may qualify for some of the expedited regulatory pathways provided by health authorities.
In the setting of ACLF, several toxic metabolites, including ammonia, may accumulate in the body due to organ dysfunctions and failures. VS-01-ACLF is designed to enhance the clearance of ACLF-related metabolites by extracting them from the blood into the peritoneal cavity by passive diffusion. Toxic metabolites, either captured by the liposomes or in the surrounding fluid, are then drained from the body. Preclinical studies and the First-in-human study have shown the potential of VS-01 as a treatment for patients with ACLF by simultaneously supporting liver, kidney and brain function.
Phase 1b First-in-Human (FIH) in Patients with Decompensated Liver Cirrhosis, Ascites and Covert Hepatic Encephalopathy
A Phase 1b first-in-human study was completed in patients with decompensated cirrhosis, ascites, and covert hepatic encephalopathy (HE), to assess the safety and tolerability of VS-01 following intraperitoneal administration of single-ascending doses and multiple doses on top of standard of care (SOC). The study demonstrated that VS-01 was generally safe and well tolerated. Preliminary efficacy assessments showed that, following administration of VS-01 on top of SOC,
- >80% of patients presented with improvement or stabilization of liver disease severity8
- ammonia was cleared dose-dependently
- cognitive assessments in patients with HE improved consistently
- plasma metabolomics associated with organ failure and infection in ACLF were reduced.
Development Stage
VS-01 is currently being evaluated in the international UNVEIL-IT® Phase 2, open-label, randomized, controlled, multi-center, proof of concept study to assess its efficacy, safety and tolerability on top of SOC compared to SOC alone, in adult patients with ACLF grades 1 and 2 and ascites. The primary objective of the study is to measure efficacy using the Chronic Liver Failure Consortium (CLIF-C) ACLF9 score at day 7.
Nitazoxanide (NTZ)
As part of our preclinical program, we have studied NTZ in in-vitro and in-vivo disease models. NTZ and Tizoxanide (TZ), its active circulating metabolite, have a broad anti-infectious spectrum acting on bacteria, viruses and parasites commonly encountered in human intestinal flora. Thus, an oral treatment with NTZ is expected to improve bacterial overgrowth and dysbiosis in the gut and possibly preserve the intestinal barrier in patients with ACLF. We also observed that, in cultured human liver cells, TZ inhibits a key pathway of programmed cell death (apoptosis) in a dose-dependent manner.
Moreover, NTZ confirmed its potential for further development in ACLF in disease models10: NTZ reduced LPS-induced inflammation in healthy rats, showed beneficial effects on liver function markers (bilirubin, albumin) in models of cirrhosis, reduced brain edema in models of ACLF, reduced inflammation markers in models of ACLF, improved survival in treatment models of sepsis, and prevented plasma increases in two renal function markers (cystatin C and creatinine).
Two Phase 1 Studies in Subjects with HI and RI
A Phase 1, open-label clinical study to evaluate the safety, tolerability and pharmacokinetics (PK) of NTZ in subjects with hepatic impairment (HI) was completed in 2022. Subjects received oral doses of NTZ twice a day for 7 days. NTZ was generally well tolerated, with a favorable safety profile. Data from a second Phase 1 study conducted in subjects with renal impairment (RI) also support a favorable safety and tolerability profile. Taken together, the Phase 1 safety and pharmacokinetic results, as well as exploratory pharmacodynamic data, support further clinical development of NTZ in patients with ACLF.
Development Stage
Following engagement with the FDA, and on the basis of the preclinical work and Phase 1 data, GENFIT has decided to pursue the development of a new nitazoxanide formulation, which will permit greater dosing flexibility to better serve ACLF patients, known to have impaired organ function or organ failure.
SRT-015
In May 2023, GENFIT licensed the exclusive worldwide rights of the ASK1 Inhibitor SRT-015 (injectable formulation in acute liver disease11) from Seal Rock Therapeutics.
ASK1 inhibition: a Therapeutic Strategy with Multi-system Benefits
Preclinical and clinical evidence support apoptosis signal-regulating kinase 1 (ASK1) inhibition as a relevant therapeutic strategy in multi-system disorders such as ACLF. ASK1 inhibition has shown several potentially beneficial effects that may be relevant in ACLF, such as blocking LPS (lipopolysaccharide) associated hyper-inflammatory response, reducing ROS (Reactive Oxygen Species)-related immune response, reducing apoptosis, reducing release of pro-inflammatory cytokines, reducing fibrosis, and protecting macrophage.
Multi-organ benefits have also been observed in several animal models and clinical trials.12 Indeed, ASK1 modulation was observed to limit renal inflammation, apoptosis and fibrosis in kidney diseases; to prevent hepatocyte death, inflammation and fibrosis in liver diseases; to limit neurodegeneration in brain disorders, to limit damaging immune responses in inflammatory diseases; and to slow onset of heart failure in cardiopulmonary diseases.
Development Stage
A First-in-Human study is planned to support the initiation of a Proof-of-Concept study in ACLF patients
CLM-022
In July 2023, we licensed the exclusive worldwide rights to CLM-022 in the field of liver disease, a first-in-class NLRP3 (nucleotide-binding domain, leucine-rich–containing family, pyrin domain–containing-3) inflammasome inhibitor, from Celloram Inc.
Primarily in animal models of liver injury and inflammation,13 studies have shown promise for NLRP3 inflammasome inhibitors in reducing liver damage and inflammation.
Development Stage
We will leverage Celloram’s scientific insights into this molecule, to finalize IND enabling studies and secure an IND for future clinical trials.
VS-02-HE
About Hepatic Encephalopathy (HE)
HE is one of the most common complications of ACLF. It is a central nervous system disorder representing a diverse spectrum of neurologic symptoms (sleep-wake cycle disturbance, fatigue, concentration difficulty, personality changes, tremor, cognitive deficits, and, in severe cases, coma), and typically occurs in patients with advanced chronic liver disease or porto-systemic shunting.
In chronic liver disease, toxins, including ammonia, accumulate in the systemic circulation and can cross the blood-brain barrier. Excess ammonia induces accumulation of glutamine in astrocytes causing osmotic stress and alteration of cell metabolism and can result in brain edema or swelling.
As many as 45% of patients with cirrhosis will experience at least one episode of HE.14 In the US only, 2 million patients are believed to be at risk of developing HE and 200,000 patients are hospitalized yearly.15 In Europe, incidence is close to 1 million patients.
Patients with ACLF and HE have higher mortality rates compared to patients who have ACLF only.16
Unmet needs
HE is largely underdiagnosed and undertreated and is associated with poor quality of life. Current treatment options for HE focus on either reducing ammonia production and absorption or on promoting its elimination by eliminating ammonia-producing colonic bacteria. Non-absorbable disaccharides such as lactulose, however, exhibit various limitations such as persistent side effects leading to poor compliance, which indirectly affects overall efficacy. The approved used of antibiotics, such as rifaximin, is limited to the reduction of overt HE recurrence rather than to the treatment of HE.
VS-02 in HE
Urease-producing bacteria in the gut are one of the main sources of circulating ammonia in humans and urease-inhibitors may represent a promising therapeutic approach for HE.
VS-02 is a hydroxamic acid (HA) derivative designed to inhibit ureases by binding to nickel atoms in their active site. We intend to develop VS-02-HE as a unique oral and colon-active formulation designed to minimize systemic absorption of ammonia and to act where ammonia is primarily produced, while reducing glutamine levels in the brain. The treatment goal is to reduce/stabilize the accumulation of ammonia in the blood and prevent re-hospitalization.
Development Stage
Investigational New Drug-enabling nonclinical studies are underway.
1 Arroyo V et al., Nat. Rev. Dis. Primers 2 (2016)
2 IQVIA market research
3 Axley P, Ahmed Z, Arora S, Haas A, Kuo YF, Kamath PS, Singal AK. NASH Is the Most Rapidly Growing Etiology for Acute-on-Chronic Liver Failure-Related Hospitalization and Disease Burden in the United States: A Population-Based Study. Liver Transpl. 2019 May;25(5):695-705. doi: 10.1002/lt.25443. PMID: 30861321
4 Kamath 2017
5 Estimates based on triangulation of data from below mentioned publications and PMR interview (Desai et al, Clin Transl Gastroenterol. (2019); Hirode et al JAMA Netw Open. (2020); Hernaez et al, J Hepatol. (2019); Mezzano et al, Gut (2022); Moreau et al, Gastroenterology. (2013))
6 F Thuluvath PJ et al., Am J Transplant. 2010, 10(4 Pt 2),1003-1019 ; Husen P. et al, Ann Transplant, 2019, 24, 242-251
7 Including HE as a therapeutic area closely associated with ACLF
8 As assessed by Child-Pugh score
9 The EASL-CLIF Consortium is a network of more than a hundred of European University Hospitals which carry out clinical investigations of the EASL-CLIF Chair aimed at performing large observational, pathophysiological and therapeutic studies to increase our understanding of Chronic Liver Failure and to improve the management of patients with cirrhosis
10 Poster presentation at the ILC 2022 (London) – EASL
11 GENFIT acquired the rights of SRT-015 for use in liver disease in which injectable therapy is intended to be administered for a period of 21 consecutive days or less, including the management of ACLF during such a period
12 ASK1 inhibition: a therapeutic strategy with multi-system benefits: Journal of Molecular Medicine (2020)
13 J. Med. Chem. 2021, 64, 1, 101–122
14 Vilstrup et al., Hepatology 2014; Poordad et al., Aliment Pharmacol Ther 2007
15 Potnis et al., International Journal of Hepatology 2021
16 Maggi DC, et al. Ann Hep 2019
